On April 8, 2021, CMS released the new Skilled Nursing Facility (SNF) Prospective Payment System (PPS) Proposed Rule which, once finalized, is effective October 1, 2021. This proposed rule updates Medicare payment policies for facilities under SNF PPS for fiscal year 2022. The proposed rule also includes information for the SNF Quality Reporting Program (QRP) and SNF Value-Based Program (VBP) for FY 2022.
See below for the most significant areas of updates:
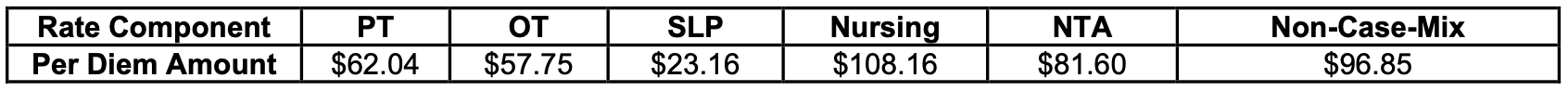
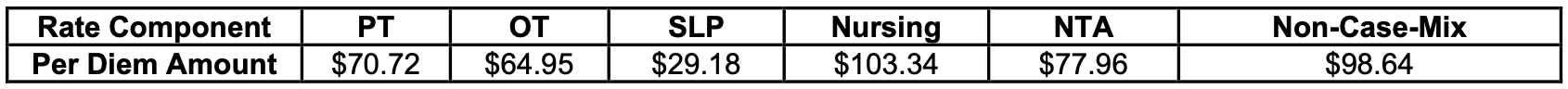
- FY 2022 updates to the SNF payment rates
- Methodology for recalibrating the PDPM parity adjustment
- Rebase and revision of the SNF market basket to improve payment accuracy under the SNF PPS
- New Blood Clotting Factor Exclusion from SNF Consolidating Billing
- Changes in PDPM ICD-10 Code Mappings – The ICD-10 code mappings and lists used under PDPM are available on the PDPM Website at: https://www.cms.gov/Medicare/MedicareFee-for-Service-Payment/SNFPPS/PDPM
- SNF QRP update – modification to the public reporting SNF quality measures
- SNF VBP Program proposal to suppress the SNF readmission measure
For more information on this proposed rule, please visit the Federal Register’s Public Inspection Desk under “Special Filings,” at http://www.federalregister.gov/inspection.aspx.