By: Sheena Mattingly, Director of Clinical Outcomes
On August 26, 2020 CMS released a memo detailing COVID-19 testing requirements. In order for nursing homes to participate in Medicare and Medicaid, staff and residents need to adhere to new testing requirements. A revised survey tool for surveyors to assess nursing home compliance in this matter is also available.
See below for a list of steps that need to be taken to remain in compliance.
1. Remember, only antigen tests and PCR tests are permitted to be used to meet the testing requirement – antibody tests are not acceptable forms of testing.
2. Testing is based on three different triggers:
Symptomatic Individual Identified
- Staff with signs/symptoms must be tested
- Residents with signs/symptoms must be tested
Outbreak
- Test all staff with previous negative results until no new cases identified
- Test all residents that previously tested negative until no new cases identified
Routine Testing
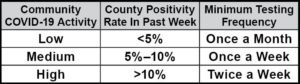
- Test staff according to County Positivity Rate in the past week
- Resident testing not recommended unless resident leaves the facility routinely
3. Routine testing must be completed of staff according to the table below and is based on the facility’s county positivity rate in the prior week. These county-level positive rates are available here (last modified Sept. 8, 2020). The below table identifies minimum testing frequency related to the county positivity rate within the past week.
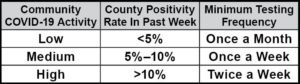
*Source: https://www.cms.gov/files/document/qso-20-38-nh.pdf
4. There is a 48-hour time requirement for results of COVID-19 testing. If for any reason, this is unable to be met, the facility should have documentation of efforts to obtain results as quickly as possible. Also, document the lab the facility is using and any contact the facility has had with local and state health departments. Criteria for the inability to meet testing result time requirements may include supply shortages, limited access, or labs failing to process tests within 48 hrs.
5. The newest F-Tag (F-866) is related to noncompliance with new testing requirements. However, if the facility has documentation supporting their attempts to adhere to new testing parameters such as timely contacting state officials and inquiries with labs that can provide results within 48 hours, then surveyors should not tag the facility. Instead, they are to inform state and/or local health departments of the facility’s lack of resources.