On December 2nd, the release of the CY 2021 Medicare Physician Fee Schedule Final Rule confirmed that we would face a huge overall 9% cut in our Med B Therapy CPT code reimbursement beginning January 1, 2021. I talked to many of you as we shook our heads and shared our mutual concern about such a large cut. The impact on our senior care providers and specifically, our rural locations would be devastating. It was clear that the outpouring of advocacy efforts in response to the fee schedule proposed rule were being ignored. During a pandemic, that has overwhelmingly impacted our geriatric population, our critical rehabilitation services were gravely at risk of not being accessible due to such significant reimbursement cuts.
Thankfully, our industry has once again proved to be irrepressible! Our associations, industry leaders, and stakeholders nationwide persevered by rallying together to fight for our rehab services to be regarded as essential and to reduce the financial impact that was imminent in the final rule. We at HTS, as an active member of NASL (National Association for Support of Long-Term Care), urged all of our therapy team members to fervently become part of the advocacy for our patients and our profession. Proudly, countless HTS employees reached out to our federal legislators to provide the necessary details of how this cut in reimbursement would affect our most vulnerable population during the PHE.
The outcry from stakeholders commanding legislative action to protect rehabilitative services paid off. In late December, Congress passed the Consolidated Appropriations Act of 2021 (H.R. 133). This provided a partial fix for the looming therapy cuts.
The overall impact to the Medicare B Therapy CPT codes was significantly diminished as a result of the provisions of this Act. Now, instead of an estimated overall 9% cut, therapy codes’ reimbursement will be reduced by approximately 3.5% (depending on the code). While this is still a financial hit in the midst of a pandemic, the ability for operators to compensate and adapt to lower reimbursement is more fathomable than the original 9% reduction. This partial fix is made possible by the following measures:
- The bill delays the implementation of the new add-on fee schedule complexity code (G2211) for three years.
- The bill infuses $3 billion into the 2021 fee schedule for one year only which adds 3.75% of payment for all codes.
- The bill delays the 2% Medicare sequester cuts for three months.
- The bill continues the current Alternative Payment Model thresholds for two additional years
- The bill extends the work 1.0 geographic index floor which increases payments for the work component of the physician fee schedule payments through December 31, 2023 for geographical areas that labor cost is lower than the national average.
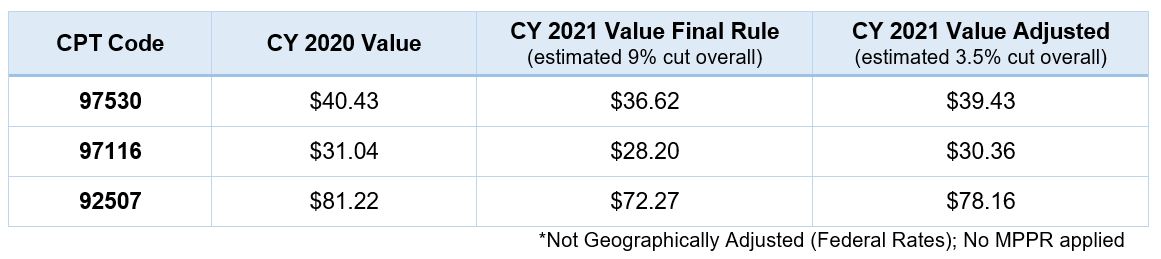
Here is an example of commonly used therapy CPT codes illustrating the impact of the Consolidated Appropriations Act of 2021 (H.R. 133) for both the 9% and 3.5% reductions.
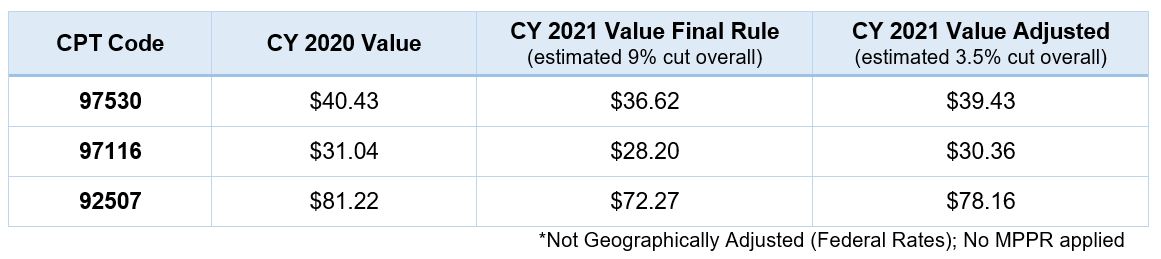
As shown in this example, providers and therapy companies alike will be challenged to offset the reduction in reimbursement. This offset may additionally be exaggerated by the overall increased costs associated with the pandemic. The need for PPE, COVID testing for employees, as well as reduced efficiencies due to isolation and other restrictions, will continue through the coming months as we continue to power through the most difficult challenge in our industry.
HTS will continue to stay steadfast during this time and true to our mission of providing “a hope and a future” (Jeremiah 29:11) to maintain the best quality of life for those we serve. Please contact me with questions, and we will continue to keep you updated on any changes on this topic and many others in the future.

Cassie Murray, OTR, MBA, QCP
Chief Operating & Clinical Officer
References:
https://rules.house.gov/sites/democrats.rules.house.gov/files/BILLS-116HR133SA-RCP-116-68.pdf
https://waysandmeans.house.gov/sites/democrats.waysandmeans.house.gov/files/documents/Overall%20Summary%20Joint%20Committees%20Final%2012.21.pdf



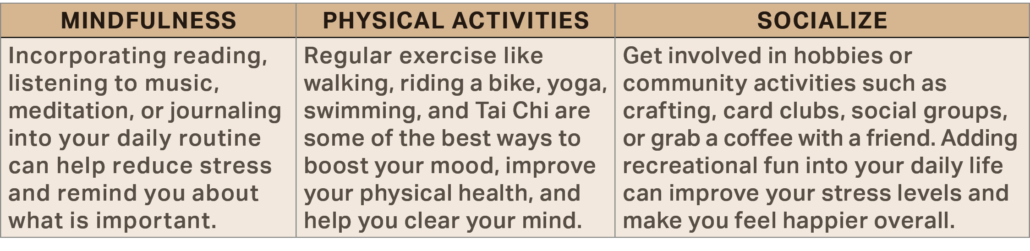
 THERAPY’S ROLE IN STRESS MANAGEMENT
THERAPY’S ROLE IN STRESS MANAGEMENT

