In today’s climate of scrutiny and burden of justifying therapy services and skilled stays, it is becoming increasingly critical for nursing to take charge in documenting each patients’ skilled needs. Specifically, what should the nurses be documenting in the medical record? How specific is the training for your nursing staff?
Before you answer, remember that the rules of documentation have changed greatly in the past 3 years. Even now, something that is the norm could likely be scrutinized in future audits. Whether you’ve had ADRs and denials for payment, it’s not a matter of if…but when. Those of us that are laser focused on the regs and changing climate of our industry know why things have altered so greatly. However, I have found that keeping to the basics is the best way to explain documentation expectations that are critical for justifying a skilled stay. I have also had my own documentation scrutinized, reviewed my fair share of ADRs and audited countless charts for congruent nursing and therapy documentation. The ideas below are a culmination of questions, mistakes, training and conversations by nurses, administrators and corporations. Try using these proven strategies to improve your skilled nursing documentation to support therapy services, and ultimately support the skilled stay:
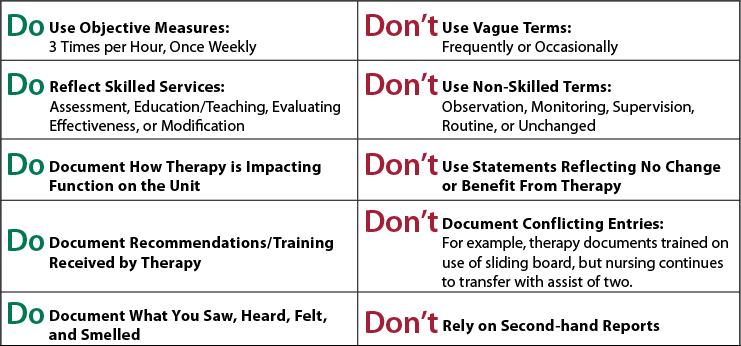
The Do’s and Don’ts:
Justifying a Skilled Stay:
Nurses must ask themselves the following questions (and document the answers) each and every day:
- Why is this patient here?
- What is preventing this patient from going home right now? Could this patient go home right now and be safe and independent? Why not?
- What are you doing that would not or could not happen for this patient at home?
- Have you noticed this patient improving in any aspect of mobility? Self-care? Communication?
*Even minor improvements need to be noticed and documented. - Why is this patient receiving PT, OT or ST?
- What would/could happen if this patient was not an inpatient receiving care?
- What are all of the medical complexities that are impacting this patient’s recovery. Explain the multiple conditions that you are managing. What is making this patient’s recovery take this amount of time?
RUG Supportive Documentation: Do they know the Why?
- Do your nurses know what a RUG level is? Try asking several nurses on your rehab unit if they know what a RUG level is…you may be surprised by how many do not know. Do your nurses understand the importance of ADL coding? Nurses need to understand the basic reimbursement system for the stay in order to understand the importance of the documentation. Provide a basic PPS inservice to help your staff understand how the MDS, nursing notes and therapy notes combined determine the RUG level. The medical record must make sense—nursing notes and therapy notes must support the coding on the MDS.
- Do your nurses understand that PLOF is critical for establishing all goals? What was the patient doing prior to the hospitalization? Was he/she completely independent with all self-care and mobility? What about higher level tasks—grocery shopping, driving, cooking, laundry?
- What does the patient need to be able to safely do prior to returning home? What impairments are preventing the patient from doing these things?
- Are your nurses documenting their skilled nursing interventions? What if therapy services are denied? Will your nursing documentation prove a skilled nursing level? Provide nursing education regarding specific skilled nursing interventions. Provide sample documentation that reflects skilled nursing interventions.
I hope that these tips and questions help to gauge the level of training and direction for our SNF nurses. Now more than ever, you deserve to be paid for the great care you provide.
HTS is committed to the success of our clients and partners. That is why we provide on-going support and education for our therapists, nurses, and the entire IDT. With the changing expectations for justified skilled stays, make sure you are partnered with a dynamic, progressive therapy provider who will support and enhance your position in our post-acute care market.
Guest Blog

Cassie Murray, OTR, QCP, IASSC CYB
Cassie Murray is the Executive Director of Clinical Services for Healthcare Therapy Services. A 1994 graduate from Indiana University in Occupational Therapy, Cassie has over 22 years of experience in long term care, hospital, outpatient and home health. She provides support for HTS therapists and partnering communities through program development, training on regulatory requirements and ongoing quality assurance. She is active in state and national associations such as Leading Age, AHCA, NASL, AOTA. Her passion for rehabilitative services is inspired from personal experience with her father suffering a stroke while Cassie was in high school. This led to her successful career path in occupational therapy.
To contact the author: cmurray@htstherapy.com | 800-486-4449 ext 210 | www.htstherapy.com