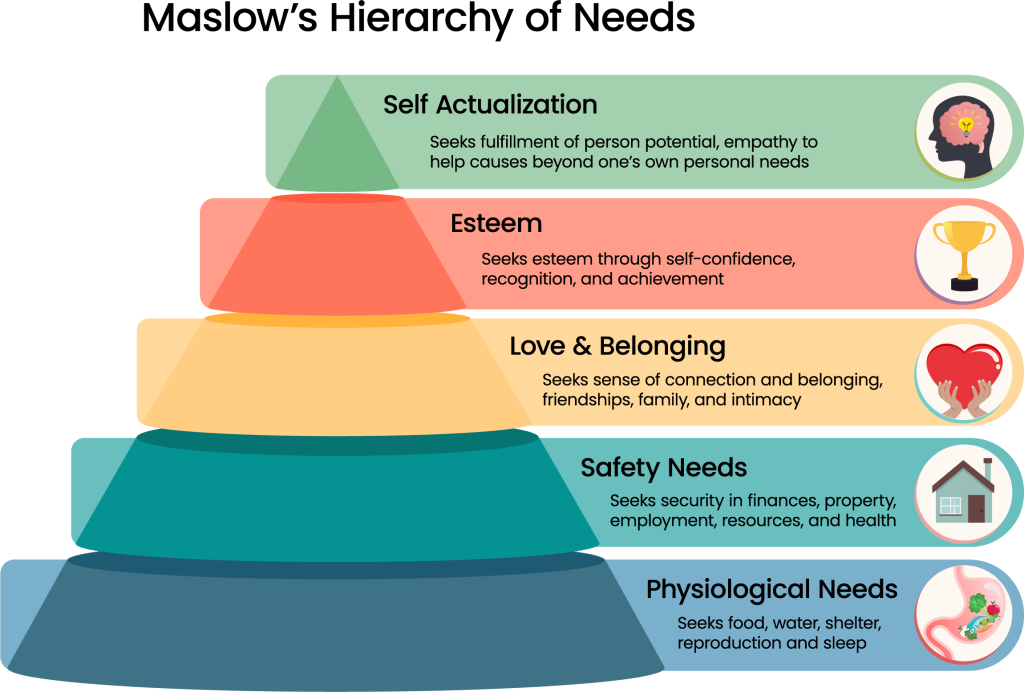
Imagine the interdisciplinary team at a SNF preparing to capture a snapshot of a patient’s readiness to “leave the nest” of the healthcare facility to return to their home. It’s a multifaceted process, assessing everything from how smoothly they move to how adeptly they tackle daily tasks.
Out with the Old. In with the New.
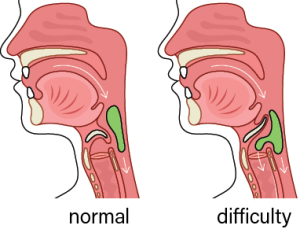
Currently, healthcare providers and therapists, armed with tools like the Functional Independence Measure or the Barthel Index meticulously assess every aspect of a patient’s functional prowess. Can they stride down the hallway? Can they complete daily tasks such as eating and oral hygiene without breaking a sweat? These scores paint a vivid portrait of their independence and self-sufficiency.
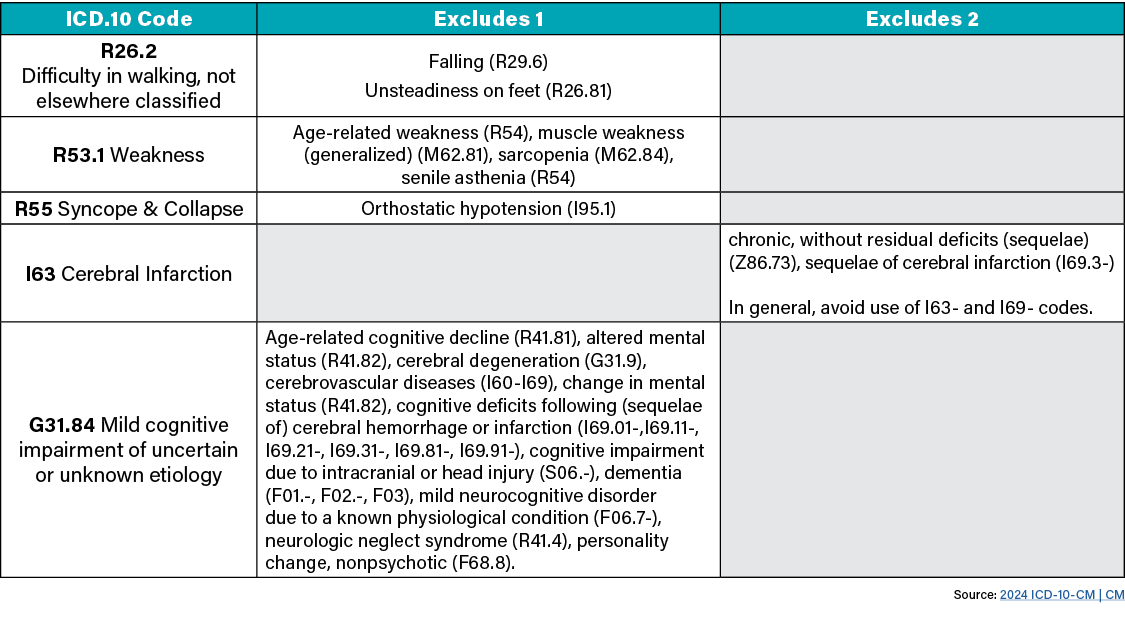
October 2024: CMS will replace the Percentage of Residents Who Made Improvements in Function (Short Stay) measure with the new Discharge Function Score measure which was finalized in the FY2024 SNF PPS Final Rule for use in the Skilled Nursing Facility (SNF) Quality Reporting Program (QRP) and the SNF Value-Based Purchasing (VBP) program. The remaining four measures will remain frozen until January 2025 while the data for the equivalent measures are collected.
The new Discharge Function Score Measure determines how successful each SNF is at
achieving an expected level of functional ability for its patients at discharge.
Why Should You Care About The Discharge Function Score?
These scores aren’t just numbers in a chart; they’re the cornerstone of how CMS will determine if the patient function is progressing in a manner that is expected and will be used in the SNF Quality Reporting Program. The final Discharge Function Score for a given SNF is the proportion of that SNF’s stays where a resident’s observed discharge score meets or exceeds their expected discharge score. According to CMS, SNFs with low scores are “not producing the functional gains they could be for a larger share of their patients.”
And let’s face it, this measure’s first year in the program is 2027 which is fast approaching. The first performance period begins FY 2025 (October 1, 2025) and everyone needs to be prepared.
The Roles of Each Stakeholder
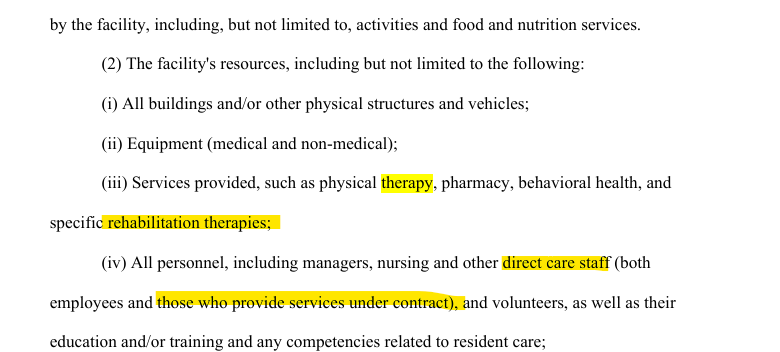
We have been preparing each therapist through the ongoing education of Section GG. HTS Therapists continually receive additional education, auditing, and coaching to ensure accuracy. Therapy will be coding Section GG as is the norm. However, this is a great time and opportunity to modify your systems so that a collaborative approach from all stakeholders is well-defined when coding Section GG on the MDS. Also, it is of utmost importance that facilities ensure information is being coded to the best of their ability. Otherwise, statistical imputation occurs and it could skew data to seem like the facility isn’t doing as well as it could have been if the information had been input as intended.
Therefore, when you hear about a discharge function score, remember—it’s definitely not just a number. It is the key to showing a SNF’s collaborative, interdisciplinary approach to rehabilitating a patient to their prior level of function as expected.
For additional information, view the CMS Discharge Function Score for SNFs Technical Reports: snf-discharge-function-score-technical-report-february-2023.pdf (cms.gov)
HTS Partners, feel free to contact me or your Regional Director for more information. As your partner in therapy, we will continue to keep you apprised of this topic along with many others.
Written by: Sheena Mattingly, M.S., CCC-SLP, RAC-CT