Exclusive PDPM Training For HTS Partners
We are committed to supporting our partners by offering exclusive PDPM webinar and live trainings in critical areas to foster success as we “Power through PDPM.”
Moving From RUG-IV to PDPM: The Transitional IPA
Wednesday, September 25, 10:00 a.m. – 11:00 a.m.
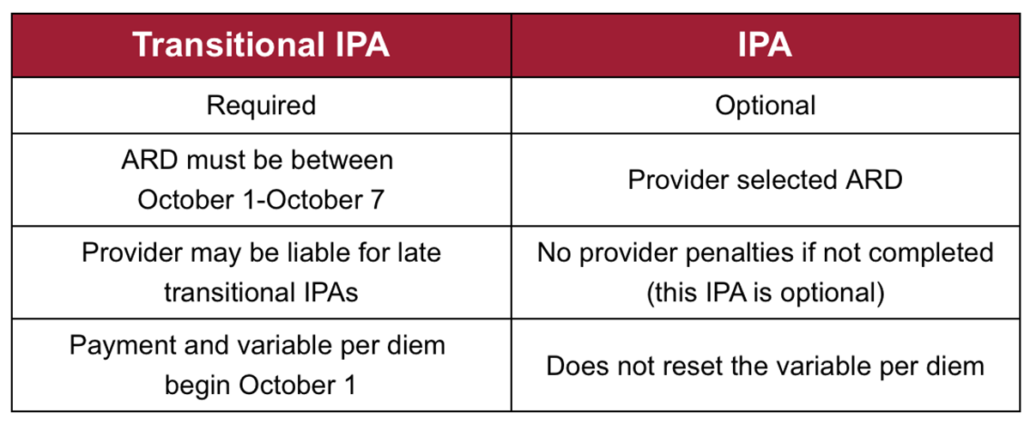
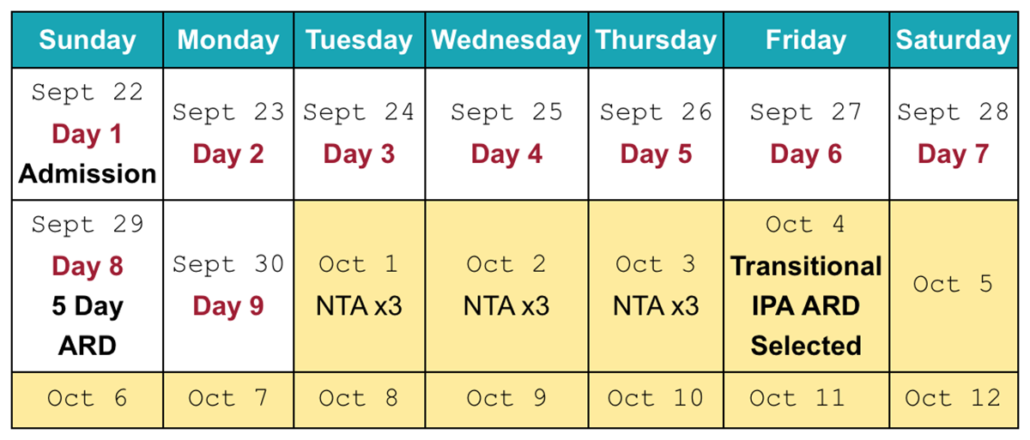
Join us for the 1st High Impact PDPM Workshop where we will review how to successfully navigate the upcoming transition from RUG-IV to PDPM. This webinar will focus on completion of the required transitional Interim Payment Assessment (IPA) for current Medicare Part A beneficiaries including gathering quality assessment data and considerations for ARD scheduling.
Presented by: Eleisha Wilkes, RN, RAC-CT
PDPM Billing Processes
Wednesday, October 23, 10:00 a.m. – 11:00 a.m.
The importance of billing accuracy becomes more important than ever under the PDPM (Patient-Driven Payment Model) effective October 1, 2019. This session will focus on tools and strategies to establish a robust Triple Check process that providers cannot afford to overlook.
Presented by: Stacy Baker, OTR/L, CHC, RAC-CT
Please contact us to register. Not a partner? Contact us to learn how we’re providing even more value to our partners.